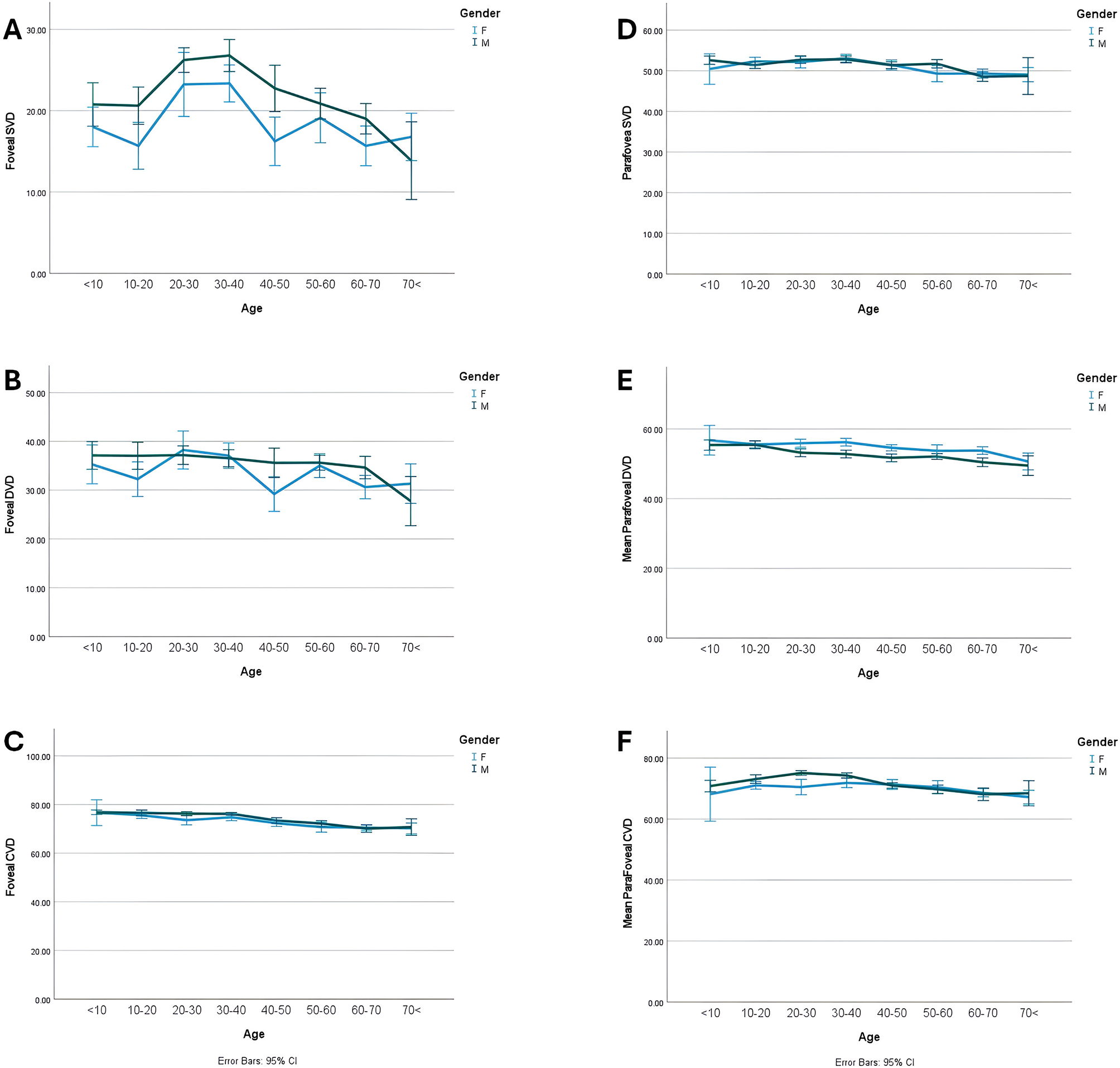
Our study found a significant relationship between age and retinal VD as well as layered RT. The overall trend of vascular densities in the foveal and parafoveal areas is a gradual decrease. However, the superficial capillary plexus (SCP) shows an upward slope until the age of 40, after which it rapidly declines in density with advancing age. Males had higher VD compared to females across all parameters except for parafoveal DVD. Like VD, age also showed a significant relationship with all total and segmental and layered RT parameters. The foveal RT chart displayed a gradual incline, while the RT in the parafoveal region exhibited an upward trend until the age of 20–30. Afterward, the slope leveled off and remained constant. RT across all layers was lower in females compared to males.
Understanding the normal values for RT and VD by OCT and OCTA helps in quickly spotting any potential issues or abnormalities [10]. We observed that at the foveal and parafoveal part, the entire RT was thicker at ages between 20 and 40. The foveal and parafoveal IRT showed the greatest level of thickness in the 20–30 age group. In the foveal area, the thickest MRT was in the fifties, and in the parafoveal area it was at age 10–20. ORT was thickest in the fifties in both foveal and parafoveal areas. The foveal and parafoveal regions exhibit the highest thickness levels between the ages of 20 and 60.
Inconsistent findings have emerged from research examining the thickness of individual retinal layers at the fovea in relation to aging. Ooto et al. revealed an augmentation in foveal RT, alongside a significantly heightened thickness of both photoreceptor outer segments and the OPL and ONL with advancing age [11]. Conversely, Demirkaya et al. identified a reduction in the retinal outer segment layer with increasing age and no alteration in the other layers of the fovea [12]. Bafiq et al. showed that the RT exhibited an inverse relationship with age, with a decrement of 0.67µmm per annum beyond the 1 mm circumference of fovea. The rates of decline in thickness differed between the inner and outer layers of the retina [13]. The process of aging has been demonstrated to be linked with the loss of neurons and glial cells in the inner layer of the retina. Examination of histological studies revealed age-related losses of 0.3–0.6% of retinal neurons per year [14]. Eriksson and Alm [15] reported a negative correlation between RT in all nine ETDRS subsegments and age. Similarly, Manassakorn et al. [16] discovered a significant association between age and macular thickness in all ETDRS areas except for the center.
Our results showed the thickest IRT in the twenties and its slowly decrease during aging. In accordance, Cavallotti et al. [17] found that RT decreases significantly with age in a histologic study. They reported a decrease in the number of ganglion cells with increased age. It appears that these cells are more susceptible to age-related loss than other retinal cells. The number of retinal capillaries, intercellular connections, cellular processes, and synaptic bodies also decrease markedly with aging. A study by Ono and colleagues [18] gives inconclusive data about the thickness of the retinal nerve fiber layer (RNFL) and does not provide good evidence of a significant correlation between RNFL and age. Nonetheless, Funaki and associates [19] reported that RNFL thickness decreases significantly with aging.
The increase in ORT in our study is not in agreement with the study of Gao and Hollyfield [20] who reported substantial progressive loss of neurons (photoreceptors) with aging. They reported that during the second to ninth decade, there was a rate of loss of equatorial RPE cells of approximately 14 cells/mm2 per year, according to their findings. We think that outer retinal thickening in our study could be due to the structural interstitial cells in the outer retina as well as the thickening of the photoreceptor’s outer segments due to structural or functional decrease in the dissolution and resorption of the photoreceptors’ outer segments. Actual changes in the overall size of the photoreceptor cells could be another culprit [17,18,19,20,21].
We found a discrepancy in the foveal area and parafoveal area regarding the thickness of MRT in the life course, as the thickest foveal MRT was in the fifties, and the thickest parafoveal MRT was in the 10–20-year group. It could be hypothesized that thickening occurs in the OPL at the fovea during time due to remodeling of foveal and parafoveal areas due to the plasticity of the retina at these areas. This layer contains the synapses between the axons of photoreceptor cells and the dendrites of intermediate neurons (bipolar and horizontal cells). An alternative hypothesis is to increase the neural or axonal content or interfibrillar glial tissue.
The other finding of our study was the correlation between all RT parameters and gender. All RT parameters were found to be significantly higher in males. However, among individuals up to 40 years, there was no significant disparity observed between males and females. Prior studies have indicated the disparities between genders and RT [22, 23]. Findings from various ethnic populations show that women have a thinner retina in the fovea and parafoveal area compared to men. Bafiq and colleagues found that females have lower RT values in both the central sub-field and the inner retinal layers compared to males. Specifically, females had a 16 μm less thickness in central sub-field thickness and a 6 μm less in IRT [13]. Notably, studies on children have shown that boys tend to have a thicker macula than girls, although some studies have reported no gender-based differences [24,25,26]. Furthermore, in another study no significant discrepancy in mean foveal thickness between men (204 μm; range, 154–232 μm) and women (207 μm; range, 173–252 μm) was detected [7]. Collectively, our findings are in line with the concept of the impact of gender on RT. The decreased thickness of the fovea in female could explain more susceptibility of them to develop macular holes. It has been proposed that macular hole formation begins with thinning of the fovea. However, further research is needed to establish the connection between hormonal effects and RT.
In the present investigation, we observed a statistical significance of the relationship between age and all VD parameters. All VD metrics indicated a decreasing tendency after the age of forty. Consistent with our results a study in 224 eyes of 112 individuals (12–67 years) showed that the VD of parafoveal and foveal areas reduced with age, but mainly in patients over 50 years old. This study concluded that, for each year of increase in age, VD of the SCP and DCP in the macula decreases by 0.32%, and 0.48%, respectively [27].
Wei et al. enrolled individuals ranging from the ages of 18 to 82 years and categorized them into four groups according to age. Their investigation revealed a negative correlation between age and retinal VD [28]. In a study by Wang et al. [29], a greater density of SCP and DCP were correlated with a younger age. Similarly, in an investigation by Yu et al. [32 − 30], on a sample of 45 healthy Chinese, observed that the mean parafoveal flow index and the mean vascular area density notably decline with age. Park and colleagues [31] showed that the densities of the retinal and choroidal capillaries, as well as the RT and CT, exhibit a tendency to diminish as individuals age, particularly after the age of 40, which is consistent with our study. Also, following age 40, the VD at parafoveal region diminished with a reduction in RT. Previously, Ding and colleagues [32] have documented a notable reduction in subfoveal CT in individuals aged 60 years and above. Additionally, Ito and colleagues [33] have reported that reductions in choroidal circulation are particularly noticeable in individuals aged 50 years and above.
Gender variations were observed in the VD across different regions of the retina among males and females. Males generally had higher VD than females, except for the VD at parafoveal area. Previous research has shown that males tend to have higher density in the SCP, while females have higher density in the DCP [29]. Also, some studies have reported higher SCP density in males [34]. Additionally, it has been noted that females, especially those over 60 years old, may have higher VD, possibly due to a slower rate of aging of blood vessels in women according to Coscas et al. [35]. In our study, females had higher parafoveal DVD.
Regarding CVI, a study by Ruiz-Medrano et al. found a significant difference in CVI levels between individuals over 18 years old and those under 18 [36]. In contrast to our study, another study, on 106 healthy eyes in individuals aged 21 to 78 years old, found that the CVI decreased as people got older. The decline in CVI was noticeable in individuals aged 33 to 43, showing a decrease of 0.7 to 2.7% per decade [37]. Our findings indicate that there is no significant variation in CVI among different age groups. The most noticeable disparities in CVI were observed at the youngest and oldest age groups. We noticed a higher amount of CVI among females in the 50–60 age group.
Our investigation possesses various advantages of a broad spectrum of age, utilization an imaging modality exhibiting good resolution of capillaries, and integration of an automated methodology for analysis. However, there are several limitations to our work. Our study used a 3 × 3 mm OCTA scan, which only roughly cover the parafoveal area. Limited by small sample size and nonlongitudinal design, our study calls for future research with long follow-up to assess repeatability of macular layer measurements of the same participants by aging. Further, understanding peripheral retinal regions and changes of macular morphology over time requires wide-field scanning methods. The influence of ethnic diversity on VD has not been assessed in this investigation. The clinical significance of the findings from this study remains to be established; however, considering the normal reduction in vascular density VD and RT after the age of 40, particular attention should be directed towards the prevalence of age-related retinal as macular holes and age-related macular degeneration, as well as specific forms of retinal dystrophies. These observations warrant validation through histological studies.
In conclusion, age was found to be significantly related to retinal VD and layered RT. Vascular densities in the foveal and parafoveal regions generally decreased, although the SCP increased until age 40 before rapidly declining. Males had higher VD except for parafoveal DVD. Foveal RT increased gradually, while parafoveal RT increased until 20–30 and then leveled off. Females had lower RT than males across all layers.

Leave a Reply