This case–control study evaluated 37 patients with CSC and BALAD and 40 patients with CSC without BALAD. The findings highlight several significant differences between these two groups, especially with the clinical characteristics and associated conditions.
One of the most significant findings was the strong correlation between BALAD and various systemic conditions, particularly psychiatric disorders (32.5% vs. 10%, p = 0.014) and corticosteroid use (37.5% vs. 10%, p = 0.032), both established risk factors for CSC. These associations suggest that BALAD may represent a more severe or complex form of CSC, potentially influenced by systemic inflammation or drug effects. Although the pathogenesis is still unclear, BALAD may result from intense force on the myoid zone of the photoreceptor inner segment to exceed the limits, leading to detachment during intense and acute subretinal exudation [3, 6, 8, 13,14,15,16,17,18,19,20,21,22,23,24].
In predisposed individuals, such as those with a psychiatric disorders and type A personality, catecholamine release can increase choroidal vessel permeability, disrupting their functional balance. Evidence also suggests that stress contributes to both the development and worsening of CSC. Stress-induced sympathetic stimulation tends to increase choroidal blood flow, promoting the onset and progression of the condition. This increase in flow may lead to focal choroidal ischemia, damaging the RPE and impairing its function. Localized ischemia can, in turn, induce greater vascular exudation, contributing to the development of serous pigment epithelial detachment (PED) and compromising the outer blood-retinal barrier, thereby intensifying the clinical presentation of CSC [28, 29].
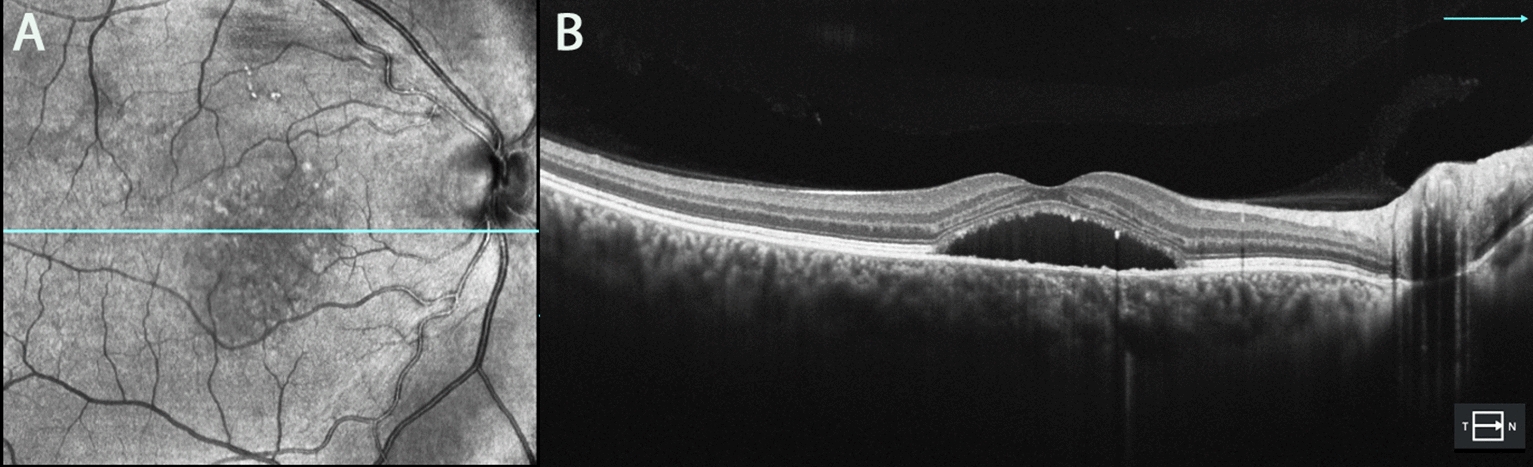
Additionally, BALAD predominantly developed unilaterally (91.4%), often localized in the foveal or parafoveal regions, and typically occurred as a single focal lesion. OCT imaging revealed distinctive features in BALAD group, including a round, yellowish foveal lesion within the neurosensory retinal detachment and increased subfoveal choroidal thickness (SFCT).
The BALAD group was notably associated with visual decline due to subretinal fluid, although there was a significant improvement in BCVA between the initial and final evaluations (Student’s t-test: 2.76, df: 23, p = 0.011; Wilcoxon test: W = 347, p = 0.005 for the control group). Initially, the BALAD group presented with a more severe form of CSC, which may have contributed to worse functional outcomes at baseline. However, both groups demonstrated significant improvements in visual acuity during the follow-up period. Further information regarding treatment requirements and long-term changes in the retinal pigment epithelium (RPE) would be crucial for a more comprehensive understanding of treatment burden and the potential for atrophy.
Consistent with our findings, visual deterioration in eyes with BALAD has previously been reported in patients with age-related macular degeneration [18, 23, 24] and has been identified as a transient condition [18, 25], as corroborated by our results. These anatomical improvements were observed with the resolution of CSC, likely due to increased choroidal blood flow and improved metabolic support for the photoreceptor inner segments provided by mitochondria [3, 10, 11, 15]. Furthermore, the rapid regenerative capacity of the inner and outer segments of the photoreceptors [3] is likely a contributing factor to this improvement.
Notably, hyper-reflective particles were observed suspended within the BALAD cavity in thirteen cases (34.2%). These suspended hyper-reflective particles are often related with BALAD [24]. While alternative explanations could not be definitively excluded, we propose that these hyper-reflective materials may represent fibrin, photoreceptor debris, septa or even mitochondrial aggregates [3, 8, 12, 14, 17,18,19, 22].
SFCT was significantly greater in the BALAD group (448 ± 105.6 µm vs. 388.0 ± 82.0 µm in the control group, p = 0.036), reinforcing the hypothesis that choroidal changes play a central role in the pathophysiology of BALAD in CSC. This thickening may be attributed to choroidal ischemia [3, 11,12,13,14,15] and choroidal inflammation [24], which are known to compromise the outer blood-retinal barrier. These changes have been documented in association with inflammatory or infiltrative retinopathies [17, 25], trauma [17], acute posterior multifocal placoid pigment epitheliopathy [12, 17], and pachychoroid-associated serous chorioretinopathy [17], and could potentially lead to BALAD.
Choroidal ischemia reduces the perfusion of the outer retina, increases hydrostatic pressure, and compromises the integrity of the outer blood-retinal barrier by damaging the RPE. This leads to nutritional stress on the bacillary layer, which relies on the choriocapillaris for nourishment and regeneration [3, 11,12,13,14,15]. In BALAD, these effects likely occur more abruptly, rapidly, and intensely. As observed in our study, this has been resolved concurrently with the resolution of inflammation and fluid accumulation [24].
We hypothesize that an intense inflammatory process and prior treatments, whether through direct or indirect injury, play a key role in the pathophysiology of BALAD. The development of BALAD may be linked to severe, acute choroidal exudation into the subretinal space, which stretches and surpasses the tensile resistance of the photoreceptor inner segments, leading to splitting of the myoid layer and its detachment from the ellipsoid zone. Chronic CSC may further predispose photoreceptors to BALAD, largely due to apoptosis of the photoreceptor outer segments. This process results from the chronic accumulation of subretinal fluid, which triggers oxidative stress and inflammation, weakening the adhesion between the RPE and photoreceptors. Such weakening can result in layer detachment as photoreceptor degeneration progresses within an inflammatory environment. Similar effects have been observed in cases following photodynamic therapy (PDT), high hyperopia, and COVID-19 infection, [7,8,9,10] where the occurrence of BALAD has been linked to severe local inflammatory reactions induced by PDT, systemic inflammation associated with COVID-19, and choroidal thickening [1,2,3,4,5,6,7,8,9,10].
Although we did not specify the treatments administered during the study period, we observed a higher proportion of patients who had previously received treatments for CSC, including photodynamic therapy (PDT) (p = 0.041; 12 out of 21 eyes were treated with PDT). PDT is commonly used in CSC management as it selectively occludes abnormal choroidal vessels, reducing fluid leakage. However, PDT is also known to provoke intense local inflammatory reactions, which may contribute to BALAD development. Fernández-Vigo et al. [7] reported BALAD in 13 out of 98 CSC patients treated with PDT, supporting its potential link to inflammatory processes. Although there is no direct evidence that PDT damages mineralocorticoid receptors (MRs), recently identified in the choroid, retinal pigment epithelium (RPE), and photoreceptors, it may indirectly affect these receptors. PDT-induced inflammation and oxidative stress could alter MR expression or sensitivity. MRs play a crucial role in choroidal water balance and vascular pressure regulation and contribute to choroidal thickening. This suggests that MRs may be vital in modulating choroidal blood flow and vascular permeability, with potential implications for retinal homeostasis and CSC pathology [26,27,28].
Similarly, patients with high hyperopia often have a thicker sclera, which can cause fluid accumulation in the choroid due to increased resistance along the vortex vein pathway, like uveal effusion syndrome. The vortex vein crosses a longer intra-scleral path, increasing the risk of blockage and outflow resistance. This thicker sclera reduces permeability and intensifies venous resistance, raising local pressure and fluid buildup. In our study, a high rate of missing exams in the case group (52.5%) compared to controls (17.5%) may bias results, potentially affecting interpretation of the association between ametropias and the condition studied [26, 27, 29].
In patients with COVID-19, exacerbated interleukin activation leads to a cytokine storm due to intense systemic inflammatory manifestations. Additionally, these patients received high doses of systemic corticosteroids, which, combined with the inflammatory state caused by the infection, may contribute to the unique characteristics observed in the disease. These cases suggest a potential association between COVID-19 infection, corticosteroid use, and the development of BALAD in susceptible individuals. People with pro-thrombotic conditions, such as COVID-19 and systemic lupus erythematosus (SLE), may experience compression of the choriocapillaris and Sattler’s layer, resulting in RPE dysfunction. This leads to the accumulation of large molecules, like fibrin, in the subretinal space, which may cause detachment and other RPE alterations [3, 6, 10, 13, 17, 22].
This study has several limitations, including its retrospective design, relatively small sample size, and lack of long-term follow-up data. The limited sample of 37 patients with BALAD impacts the statistical robustness and generalizability of the findings. With a smaller sample, there is a higher risk of bias and reduced statistical power, which makes it challenging to detect subtle associations or differences between variables. This may result in findings that are not fully representative of the broader population, thereby limiting the reliability of the conclusions. Furthermore, individual variability has a greater influence in smaller samples, meaning that individual differences can disproportionately impact the results compared to larger samples, where such variations tend to balance out. To mitigate these limitations, we implemented adjustments to control for potential confounding factors by matching cases with controls of similar age and disease severity. These adjustments improve the precision of our estimates and the internal validity of the study, making the findings more reliable despite the sample size limitation.
Another limitation is the lack of data on axial length and refractive status for all eyes, which may hinder our assessment of the relationship between CSC and BALAD (bacillary layer detachment). Factors such as hyperopia can alter choroidal circulation dynamics, potentially influencing susceptibility to BALAD. Without this information, it is more challenging to fully understand the role that these anatomical variables play in BALAD development in CSC patients, limiting our ability to determine if BALAD occurs more frequently in specific ocular profiles.
Although, to our knowledge, this case–control study appears to be the largest in the literature concerning the rare disease of CSC with BALAD (PubMed search, July 2024).
In conclusion, the BALAD group highlights the significant role of inflammation in the association with CSC, suggesting that BALAD could serve as a potential biomarker, even though the precise role in chronic CSC remaining unclear. The findings suggest that the BALAD group experienced a more severe condition, characterized by a higher incidence of comorbidities, more aggressive or ineffective prior treatments, and less favorable initial clinical characteristics. These results reveal distinct ocular changes, broadening the spectrum of CSC presentations and enabling differentiation from other similar macular diseases. Additionally, this study emphasizes several clinical implications, including notable choroidal thickening and significant correlations with corticosteroid use, psychiatric disorders, and prior treatments, particularly photodynamic therapy (PDT).

Leave a Reply